Harmonizing the Gut-Brain Axis: A Holistic Approach to Understanding and Treating IBS

The Effects That The Gut Microbiome play on our Stress and Enteric Nervous System and How to Modulate These With Somatic Based Therapies.
Where does the ‘Irritable’ in Irritable Bowel Syndrome come from?
Hyper Visceral Sensitivity in IBS
Patients with IBS tend to also have something called Hyper Visceral Sensitivity, or sensitivity to the viscera or gut sensations around the GI area. This may be due to the sensation’s ability to activate the nervous system, particularly the Enteric Nervous System which is responsible for activating the body and brains “alarm system”.
The Enteric Nervous System’s Profound Connection
Also, the degree that the Enteric Nervous System is connected to gut may be more proficient than you think. The body is a bio-intelligent organism that processes 40 million bits of data per second but prefrontal cortex or cognitive brain is only able to process 40 bits of information per second, so our body can be seen as a part of our subconscious and holds a lot of the trauma for us.
Cognitive Behavioral Therapy and Beyond
Addressing the Autonomic and Enteric Nervous System
While methods like Cognitive Behavioral Therapy primarily work mostly on the prefrontal cortex, the autonomic and enteric nervous system must also be addressed. Our prefrontal cortex is what makes humans human as it is the latest addition to the brain evolutionarily speaking.
The Role of Ancient Brain Centers
Animals mostly use other more ancient parts of their brain such as the amygdala and the brain stem. In a sense, the prefrontal cortex is too new, and to work with the nervous system we need to access these more ancient centers of the brain.
The Challenge of Self-Calming
This is why it may be hard to tell yourself to simply “calm down” during a flare up or panic attack. Likewise, it may be hard to calm a barking dog down by doing the same.
Understanding the Dog’s Perspective
A dog’s prefrontal cortex is not as developed as ours and can have trouble understanding words since its capacity for language is limited. Unless if you say “calm down” in a very soft manner, or go over and physically pet the dog, a language the dog’s nervous system can understand, the dog will remain barking.
Applying This Understanding to Human Anxiety
This is because the dog is functioning more from its ancient counterparts such as the amygdala and brain stem, and not its thinking mind like we do. Similarly, this is also what we must do to our own bodies to help ease certain anxiety disorders and the “Irritable” in Irritable bowel syndrome.
Somatic Therapy and Its Role in Treating IBS
So how do we help the nervous system calm the gut down? Peter Levine (fun fact: his brother was the one who discovered Endorphins), is an author, psychotherapist and founder of Somatic Exepriencing. He went through his own trauma and invented a new form of therapy to help himself and others. He called this Somatic Therapy.
The Concept of “The Container”
In Somatic Therapy, the body is called “the container” because it’s where we store all our emotion and trauma. So instead of working with the thinking rational cognitive brain, we need to delve deeper into “the container” and the networks connecting it to the brain.
Addressing the Autonomic and Enteric Nervous System
Thus, the autonomic and enteric nervous system need to be taken into account when talking about more body-based problems such as hyper visceral sensitivity and gut issues. When we get scared, our survival mechanism tells us to go into sympathetic or fight or flight nervous system, which then halts digestion so we can run away from nearby threats like a lion chasing us.
The Impact of Stress on Digestion and Gut Health
This then decreases peristalsis and then can further increase SIBO (or LIBO) and other gut issues if we remain in this state for too long. So when our bodies are stuck in sympathetic or fight/flight and our rumination keeps us in a cycle, we can start to notice the bad effects this has on the nervous system and our gut.
Why Zebras Don’t Get Ulcers
Hence Robert Sapolsky’s book titled Why Zebras Don’t Get Ulcers. Animals, like the zebra, can turn off their sympathetic and go back into safety mode automatically without thinking about it even after getting chased by a lion and seeing their friend get captured and eaten.
The Role of the Body’s Fascia and Interstitium
The trauma and stress also have an impact on our bodies’ fascia, the band of connective tissue that wraps around our entire body. This and the interstitium, the fluid-filled spaces in tissue that are connected throughout the body which neuroscientist believes holds consciousness, can also have an impact on our neurophysiology.
The Gut-Brain Connection: A Two-Way Street
So as you see, the body plays a large role in what is going on in our mind and guts, but as you will find out, the gut and mind are almost inseparable and should almost be considered as one entity.
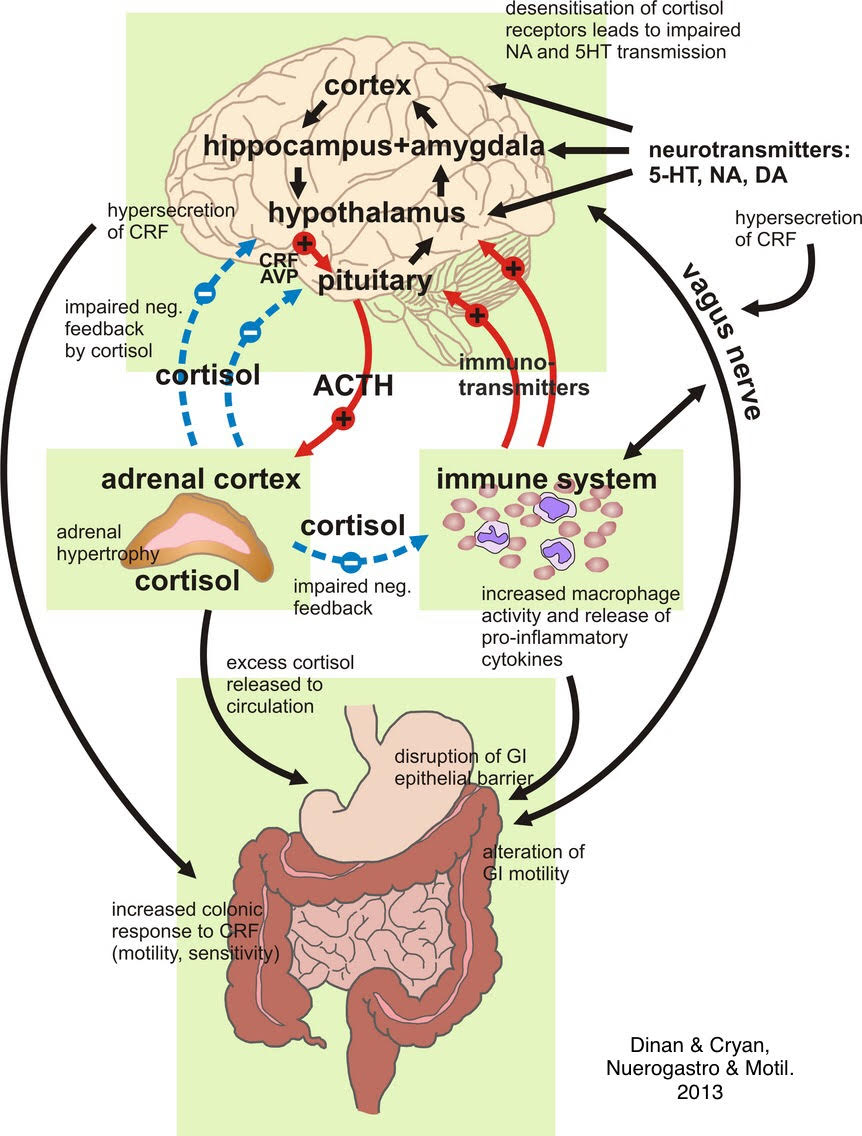
The Vagus Nerve: A Critical Link Between Gut and Brain
One can’t mention the gut-brain connection without mentioning the vagus nerve’s connection between the two. “The vagus nerve acts as a vital metabolic signal relay between the brain and the abdominal viscera. The effects of gut-based vagus nerve transmission on higher-order cognition domains, such as anxiety, depression, motivation for rewards, learning, and memory, have recently been discovered in both rodent models and humans.
Vagal Afferent Transmission and Its Effects
Consuming food activates vagal afferent transmission that originates in the gastrointestinal system, reducing anxiety and depression symptoms while enhancing motivation and memory. This procedure encourages the storage of information related to meals in the memory, making subsequent foraging activities easier.
Pathological Illnesses and Vagal Tone Regulation
The topic of vagal tone regulation is also covered in relation to pathological illnesses including transcutaneous vagus nerve stimulation for phobias, major depressive disorders, and memory problems linked to dementia. These results demonstrate the significance of gastric vagus nerve signals in controlling neurocognitive functions and shaping adaptive behavioral responses.”
The Composition of the Vagus Nerve
The vagus nerve which connects body to brain and runs through the intestines is composed of 20% efferent fibers which sends signals from the brain to body and 80% afferent sensory fibers which carries information from the body to the brain. Dianna Funes, clinical coordinator of the microbiome center UCLA, is running a study on CBT affects on gut.
The Importance of Body-Based Modalities
I do believe in top-down approaches as organizing the mind can lead to a calmer body. However, since 80% of sensations are coming from the body up, we also must take into account the vagus nerve and enteric nervous system. CBT will help but it will be more helpful to do it in conjunction with these more body-based modalities when talking about any hypersensitivity in the body at any degree or if CBT is not getting you any results.
Understanding Polyvagal Theory in the Context of IBS
To put it in terms of Stephen Porge’s Polyvagal theory, once the gut becomes hyperactive, so does the ENS and ANS, perpetuating a cycle where any sensation in the gut can bring you from the “ventral vagus” (calm and collected) state on the Polyvagal chart to the “sympathetic fight/flight” or even “Dorsal vagus” (shut down state or freeze).
The Impact of External Threats on the Nervous System
Think if you are camping having a nice night you are in a calm and collected ventral vagus state. However, if a bear approaches your body instinctively goes into fight/flight/freeze. In other words, you might try to fight the bear, run away, or freeze if you feel the situation is hopeless, you’re too scared to move, or think that it might be better to play dead to see if the bear will leave you alone. If you stay in this for too long you will expend too much energy and eventually shut down and go into “Dorsal Vagus”.
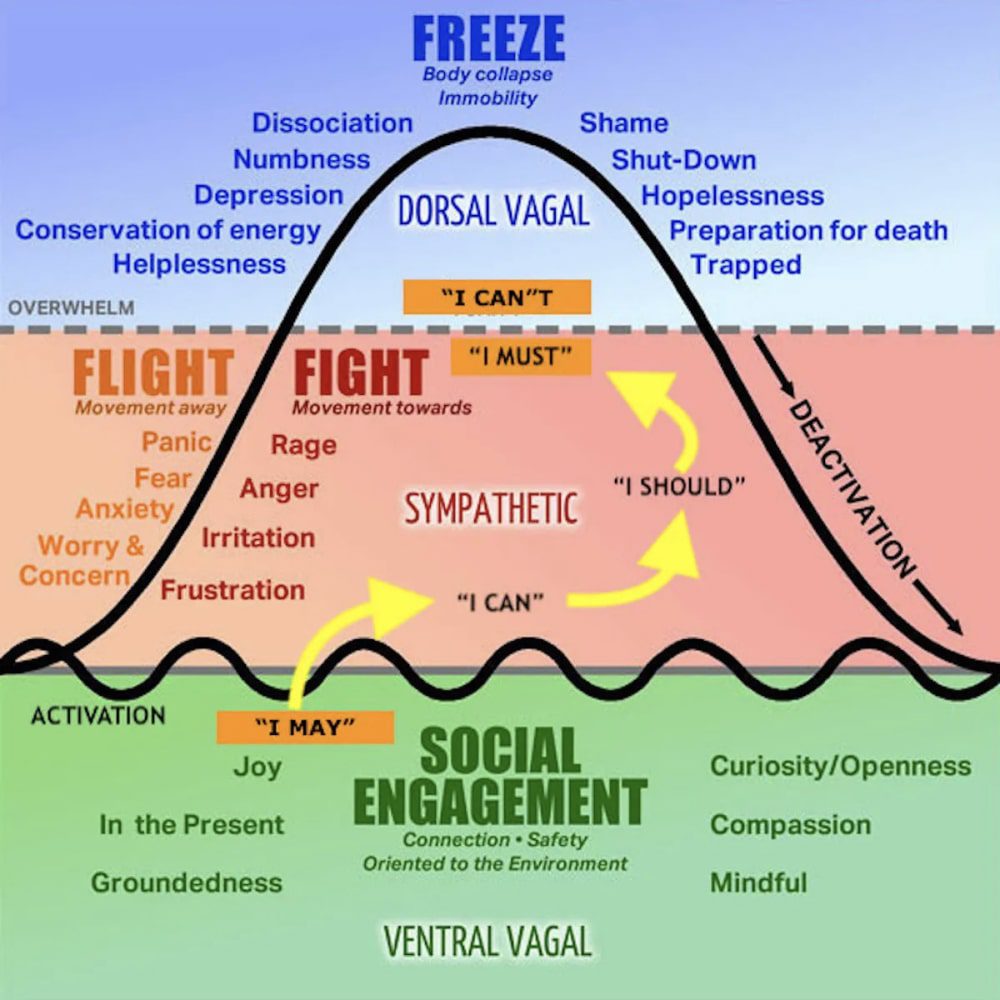
The Feedback Cycle of Hyper Visceral Sensitivity
This only further perpetuates the hyper visceral sensitivity sending the patient into a feedback cycle of sensation in the gut to paranoia and anxiety in the brain and back and forth. Their threshold or ability to stay calm in ventral vagus instead of going to Sympathetic is altered the more the gut is in dysbiosis.
The Gut-Brain Axis and Behavioral Responses
“Several studies have focused on the bidirectional communication that takes place between the gastrointestinal tract and the central nervous system (CNS). Previous studies have revealed the major role gut microbiota have on brain function, and consequently, neuropathology. Anxiogenic affective-like behaviors are lower in mice that exhibit increases in specific genera, including Lactobacillus and Bifidobacterium, and these changes were linked to altered neural function. A similar relationship between Bifidobacterium and anxiety in humans has been established.”
The Influence of Diet on Mental Health and Behavior
This may be why you see more irrational and sometimes even violent, aggressive behaviors in patients with dysbiosis. We have seen poor diets related to mental health patterns including even violence and crime. “One hypothesis suggests that food types, nutritional impact, and psychological–behavioral responses are linked to reducing crime. Nutritional impact plays a crucial role in brain function and neurotransmitter production, influencing behavior and mood. A balanced diet incorporating foods rich in micronutrients, like fish, is associated with lower aggressive behavior rates. High-fat and -sugar diets can affect brain neural pathways, potentially leading to withdrawal symptoms and behavioral changes.”
Exploring the Link Between Gut Health and Psychological Well-being
It would be interesting to do a study with Heart rate variability with dysbiosis patients and non-dysbiosis patients put in a stressful situation. The non-dysbiosis would probably score better because dissociation from the body and ENS would be altered dramatically. Try going up to a patient and touching their gut without their permission, there will most likely be a jump scare due to hyper visceral sensitivity. This is because of the ENS altering the gut and the gut altering the ENS and therefore the brain. Recording the microbiome before and after would also lead to interesting results. Important to note that the threshold of the participant with dysbiosis would be far less than someone without dysbiosis just because of the prolonged hyper visceral sensitivity. Remember the bacteria in our guts are making a lot of our neurotransmitters for the brain.
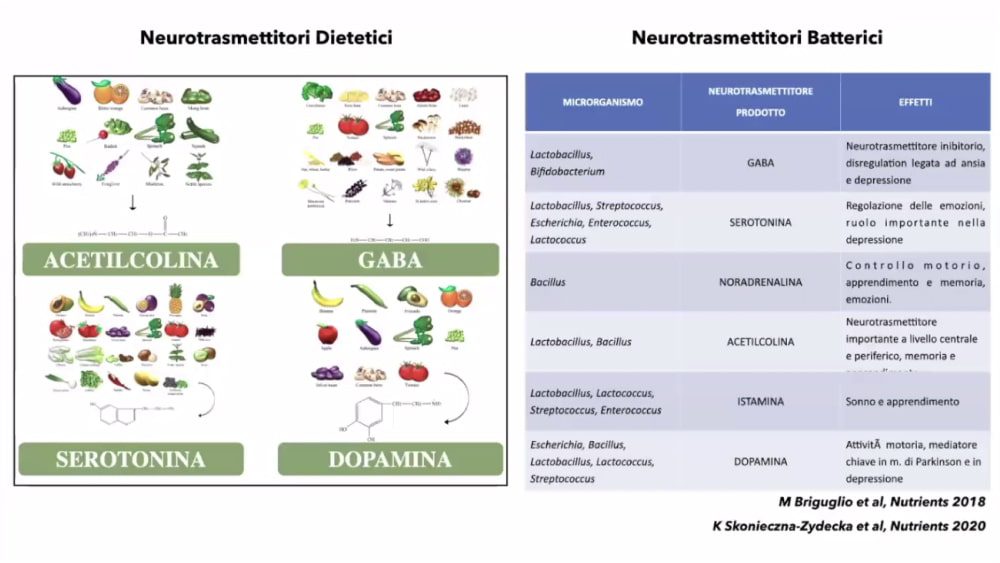
The Role of Gut Microbiota in Neurotransmitter Production
The less bacteria you have in the gut, the less support of ANS and ENS, which means entering into a state of sympathetic fight/flight becomes easier. Also, a state of sympathetic NS and dorsal vagus shuts off our prefrontal cortex, our reasoning part of the brain, which leads to irrational decision-making. So to clarify, a person with a high, abundant variety of good Prevotella, Bacteroides, Firmicutes species will have a better threshold for anxiety than a person with a high Proteobacteria, pathogenic E. Coli (bad species) gut.
Impact of Gut Health on Personality and Stress Response
Take for instance this study on SIBO, “The present study indicates that patients with bacterial overgrowth in the small intestine showed higher levels of neuroticism and lower levels of extroversion than those without this disorder. The SIBO subgroup had higher situational anxiety and stress, both overall and at the level of the three indicators: emotional tension, external stress, and intrapsychic stress. It was also shown that, in the SIBO subgroup, extroversion was lower than that in the non-SIBO subgroup and correlated with higher stress (particularly emotional tension). Knowledge of the gut-brain axis effects on SIBO pathophysiology and personality can help identify medical and psychological CBT psychotherapy treatments for stress reduction under these conditions.” The person with a better gut microbiome will perform better in stressful events. If the microbes are making our neurotransmitters, then this can also help people with depression by providing more precursors to their serotonin or dopamine. It would be useful to consider probiotics in regards to the psychological setting as well.
Integrating Somatic Therapy for PTSD and Gut Health
A combination of Somatic Therapy can also help with those suffering from PTSD. According to a study from Internal Medicine Journal, “veterans with PTSD were up to 81% more likely to undergo colonoscopy than veterans without PTSD.” Why do 81% of PTSD vets feel these sensations in their gut? It could be because the body stores all this emotional information. Especially if when the situation that caused the PTSD was too much for their mind at the time. It would be useful to, when he/she is ready, to get in contact with that “energy” in the body and to help modulate with probiotics as a therapy. We do not have a word for this “energy” besides “sensation” or “feeling” but I like to put it in the likes of an Electromagnetic Field that maybe once we have the right tools can be observed but for now, we will have to go with what the person suffering from PTSD describes it as. Therefore, body-based modalities like somatic therapy could be helpful alongside CBT for gastrointestinal issues. Some modalities include yoga, neurofeedback, breath-work, progressive muscle relaxation, sensorimotor psychotherapy, TRE, EMDR, PEMF, rolfing, fascial maneuvers, cranial sacral, tapping, qi gong, tai chi, etc. A lot of modalities trauma specialist and author Bessel Van Der Kolk recommends in The Body Keeps Score would work as well. Peter Levine also gives exercises at the end of all of his books to try. Even smelling lavender would work because that is connecting to the amygdala or olfactory sense instead of the prefrontal cortex, cognitive brain. Pretty much anything that connects you to your body while you notice the sensation helps. Even standing on one leg.
The Importance of Self-Awareness in Managing Anxiety and Gut Health
You have to have enough self-awareness though to see this. That’s the key. And self-awareness in the moment. Not after the fact, although after the fact is still helpful. Eventually, you’ll get good enough to notice when there’s anxiety or a panic attack caused by bodily sensations or the gut that you’ll be quicker to notice. This is hard when everyone is on their phone or distracted by constant media which means constant hits of dopamine. Dopamine is a hormone in the brain responsible for rewards and the precursor to the catecholamines, norepinephrine, and adrenaline. So just from iPhone and constant bombardment of dopamine-derived activities alone such as high sugar meals for example, people are getting spikes in their catecholamine production or adrenaline which can’t be good for the gut. Especially with high meat intake which has the amino acids that also has precursors that can also lead to the catecholamine production. Therefore, unplugging would be useful as well as getting in touch with nature which automatically has a calming effect on the nervous system.
Fecal Microbiome Transplants: A New Frontier in Treating Gut-Brain Axis Disorders
Another therapeutic, useful agent can be Fecal Microbiome Transplants. Take for instance this study using rats with hyper visceral sensitivity. “The effect of faecal microbiota transplantation from viscerally hypersensitive DNBS-treated and naive donors was evaluated in control rats after an antibiotic-mediated microbiota depletion. Faecal microbiota transplantation from DNBS donors induced a long-lasting visceral hypersensitivity in control rats. Pain threshold trend correlated with major modifications in the composition of gut microbiota and short chain fatty acids. By contrast, no significant alterations of colon histology, permeability, and monoamines levels were detected. Finally, by manipulating the gut microbiota of DNBS-treated animals, a counteraction of persistent visceral pain was achieved. The present results provide novel insights into the relationship between intestinal microbiota and visceral hypersensitivity, highlighting the therapeutic potential of microbiota-targeted interventions.”
The Therapeutic Potential of Fecal Microbiome Transplants (FMT)
6. By using a FMT, we can restore those probiotics that were depleted in stressful situations and maybe help reverse PTSD symptoms. Take for instance, the effects on the enteric nervous system by being germ-free. “GF rats have been used to demonstrate the impact of the microbiota on migrating myoelectric complex (MMC) activity, though no change in ENS neurochemistry was observed following colonization of these animals (Husebye et al., 2001). More recently, the early postnatal developmental trajectory, neurochemical profile, and function of the ENS has been investigated in GF mice (Collins et al., 2014, Lomasney et al., 2014b). In the context of myenteric nerve fiber density, a GF environment significantly decreased the development of enteric neural networks in a region-specific manner on postnatal day 3 relative to both offspring born in a specific pathogen-free environment or to dams colonized with a simplified microbiota.” 7. This also shows that a lack of microbes in the large intestines plays a huge role in stress. Therefore, a high-quality probiotic, with a plethora of different strains, can be highly beneficial for stress, whether in the brain or body.
Conclusion
Changing Perspectives: How Gut Health Influences Our World View
To conclude, what happens to traumatized people is their entire world changes to become much more dangerous than the average person, even if just perceived. Thoughts then can arise and perpetuate this cycle which acts as wind during a forest fire making the destruction spread physiologically making the situations worsen. So CBT can take care of those thoughts, but we need to go beyond that. We need body-based modalities as well and since we know a lack of microbes in the gut can further anxiety we must also include probiotics as a form of therapy to help calm the body down as well.
The Holistic Approach to Healing: Mind, Gut, and Body
So, as the gut changes for the better, the physiology changes, the brain changes, the mind changes, the thoughts change, your overall perceived outlook of the world changes, making things far less dangerous than they were before, deactivating the sympathetic arousal, which vice versa, has a calming effect on the gut making the gut maintain homeostasis and returning it to a baseline. Therefore, changing your gut changes your world.
Citations:
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10490081/
- https://www.mdpi.com/2072-6643/11/8/1900
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10490081/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9819554/
- https://pubmed.ncbi.nlm.nih.gov/34393197/
- https://onlinelibrary.wiley.com/doi/full/10.1111/imj.16088
- https://www.sciencedirect.com/science/article/pii/S0012160616301518
Join Kefir Club
Like our probiotics, our emails are clean and good for you. Spam Free. Unsubscribe anytime.